Malignant melanoma - symptoms, risk factors, prevention and when to respond
Malignant melanoma (melanoma) is a skin cancer of melanocytic origin. Although less common than other skin cancers, it is considered the most aggressive. This guide explains in an accessible way what to look out for and how to build healthy skin protection habits. It is not a substitute for medical advice or diagnosis, but it will help you understand the key warning signs and early response options.
What exactly is melanoma?
Melanoma occurs when skin pigment cells (melanocytes) multiply uncontrollably. It can develop both within an existing nevus and on previously unchanged skin. Early notice of abnormal features of a skin lesion is crucial for a quick response.
Melanoma risk factors - who should be especially vigilant?
The risk is not equal for everyone. Below are the factors that the literature most often links to an increased risk of developing melanoma. Their occurrence alone does not determine anything, but it does inform who is particularly worthwhile to implement regular self-observation and prevention:
- UV exposure - intense sun, frequent burns (especially in childhood), solariums.
- Complexion and skin type - very light skin, freckles, light hair/eyes.
- Numerous ne vi - many nevi (e.g., >50) or atypical nevi.
- Family history - cases of melanoma in first-degree relatives.
- Age - risk increases with age, although melanoma can also occur in young people.
- Immunosuppression - weakening of the immune system.
Warning signals on the skin: what to look out for?
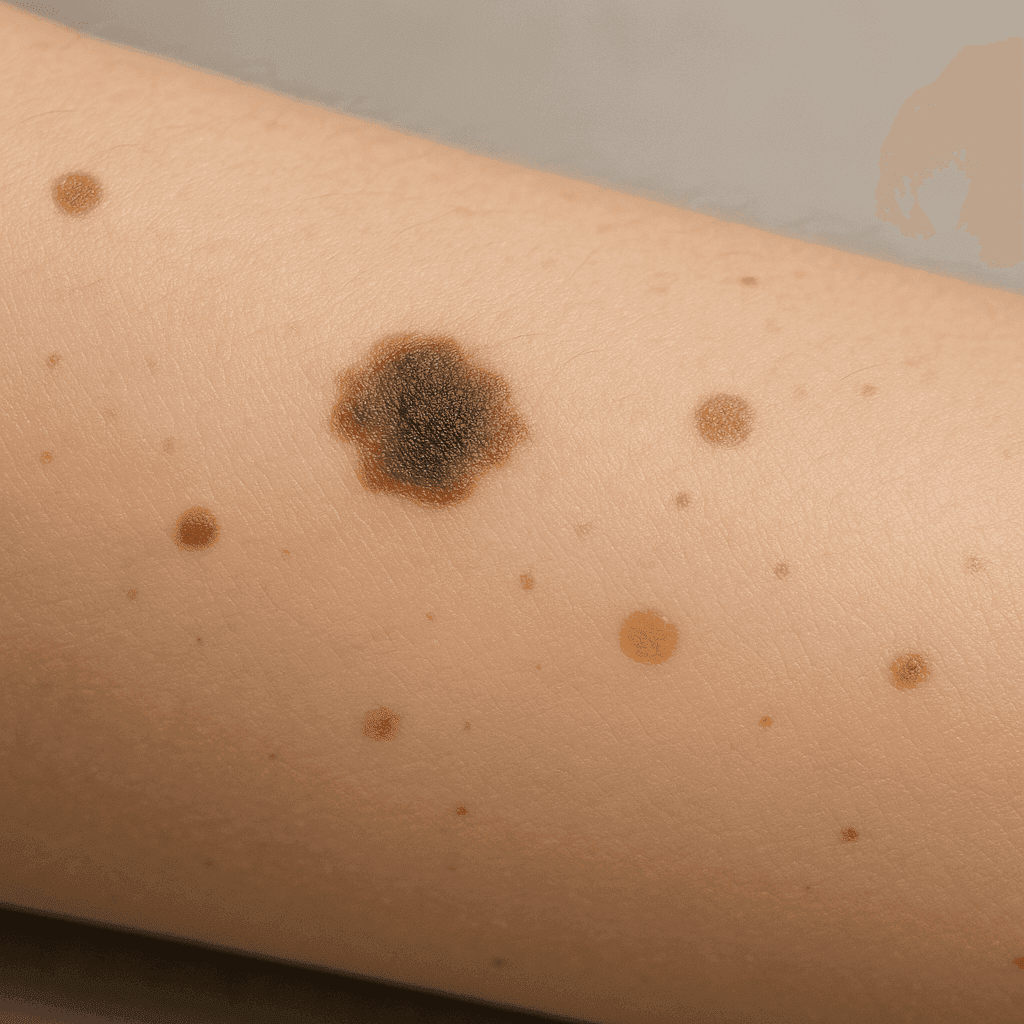
Most nevi are benign. However, it is worth paying attention to features that are often mentioned as "red flags." They do not equate to a diagnosis, but are a good reason to take a closer look at the lesion and consider a consultation:
- Asymmetry - one half of the nevus does not match the other.
- Edges - frayed, uneven, "ragged".
- Color - multiple shades within one lesion (brown, black, red, sometimes white, blue).
- Diameter - about 6 mm or more (although smaller ones may also require attention).
- Evolution - change in appearance over time (size, shape, color, associated symptoms).
This is a popular "ABCDE" mnemonic.
How do you respond when you notice a worrisome change (without making a diagnosis)?
Don't interpret the result alone as conclusive. Simple organizational and preventive steps work well in practice:
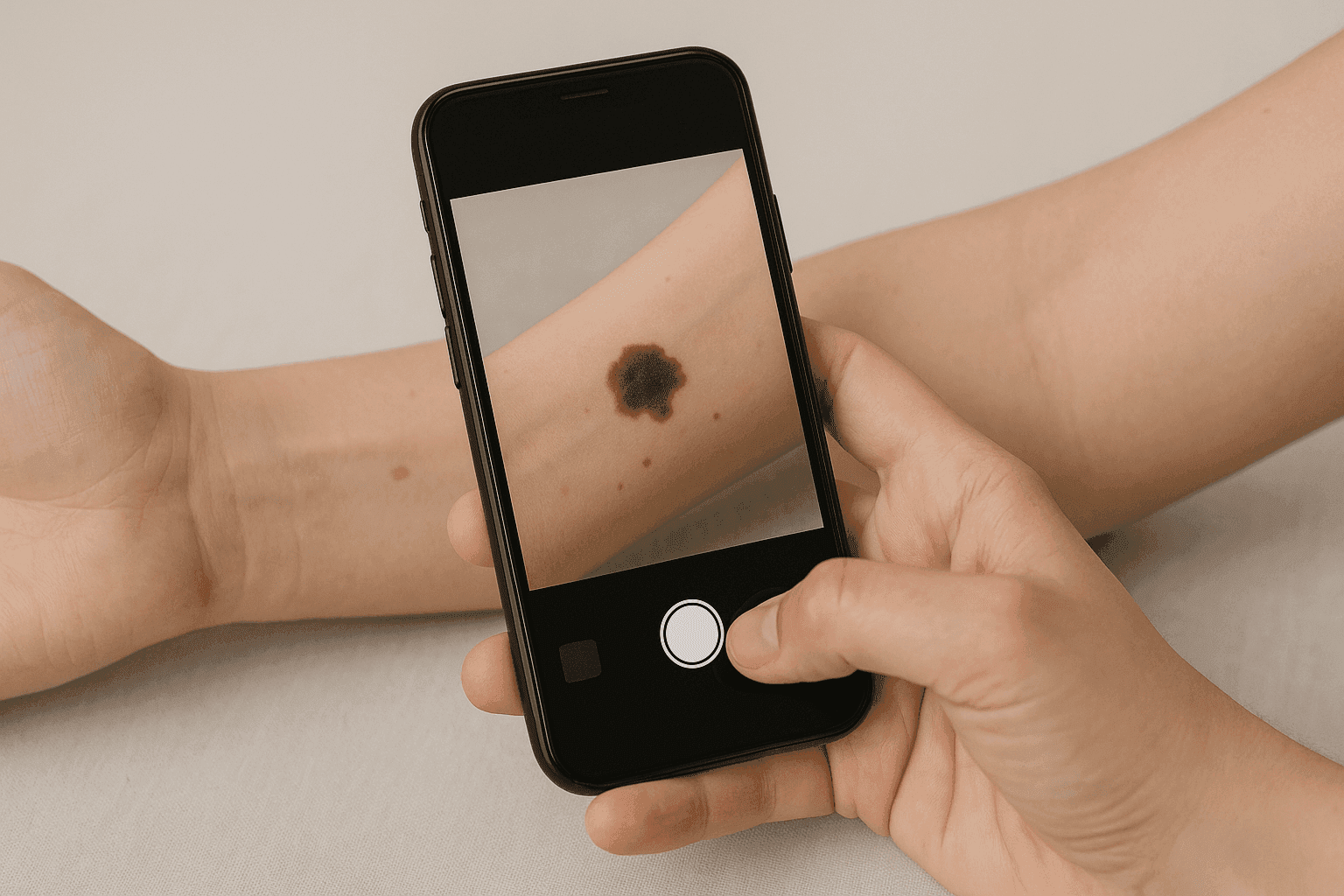
- Document the change - take a clear photo in constant light and the same distance to compare appearance over time.
- Pay attention to "new" and "other " - a new change that "doesn't fit" with the rest ("ugly duckling sign") deserves extra attention.
- Prioritize - if you notice rapid changes, don't put off further evaluation.
- Take advantage of digital tools - such as the app.medmetrix.co.uk
Prevention every day - habits that support skin health
Prevention is all about consistency and reason. Here is a set of simple habits with high practical value:
- UV protection - plan outdoor activities taking into account the intensity of the sun; choose shade and long-sleeved clothing/hats.
- Sunscreen - apply according to the manufacturer's instructions and remember to reapply, especially after swimming or heavy sweating.
- Self-check - periodically look at your skin (including scalp, feet and back with the help of a loved one).
- Plan for "high risk " - if you have multiple nevi or risk factors, set your own skin viewing schedule and stick to it.
- Document - photos are your archive - they help you spot subtle changes.
When is it especially worth expediting a consultation?
The following situations are often treated as signals for a faster response (this is not a "diagnostic" list, but a practical signpost):
- The lesion is growing rapidly, darkening or bleeding steadily.
- There is pain, itching or hypersensitivity that was not there before.
- You notice a nevus that is "completely different" from all the others.
- You have significant risk factors and concerns about a particular lesion.
The most common myths about melanoma - and how to recognize them
- "Only very dark moles are dangerous." A lesion with irregular color or asymmetry, regardless of shade, may also be of concern.
- "If a mole has been around for a long time, it's safe." What is important is the evolution over time, not the mere "presence for years."
- "Melanoma appears only on tanned skin. It can appear in different places, even less sunny ones.
- "The young don't get melanoma." Age affects the risk, but does not give full protection.
FAQ - the most common questions.
Is every irregular birthmark a melanoma?
No. Many lesions with an unusual appearance remain benign. However, irregularity can be a signal that it is worth taking a closer look at the lesion and considering a consultation.
How often is it worth looking at the skin?
Regularly and repetitively - so as to notice changes in appearance over time. People with more nevi often opt for more frequent self-examination and photo documentation.
Mini-checklists to make things easier
Home self-observation checklist
- Once in a set cycle, look at your skin "head to toe" (also scalp, behind the ears, feet).
- Note any new or rapidly changing changes.
- Take comparison photos (same distance, same lighting).
Checklist for sunny days
- Scheduled exposure (seasons of less sunshine).
- Protect yourself with clothing and accessories (hat/hat, sunglasses).
- Regular use and reapplication of cosmetics with UV filters as instructed.
Summary
Malignant melanoma is a disease that requires vigilance and regularity, but remember - many alarming signs turn out to be harmless in the end. The most important thing is to notice changes and react wisely: document, compare over time, and when in doubt, reach for supportive tools.